Oklahoma hospitals could face an $873 million annual reduction in Medicaid reimbursements under a proposed Senate bill that hospital leaders warn could devastate healthcare access statewide and force thousands of job cuts.
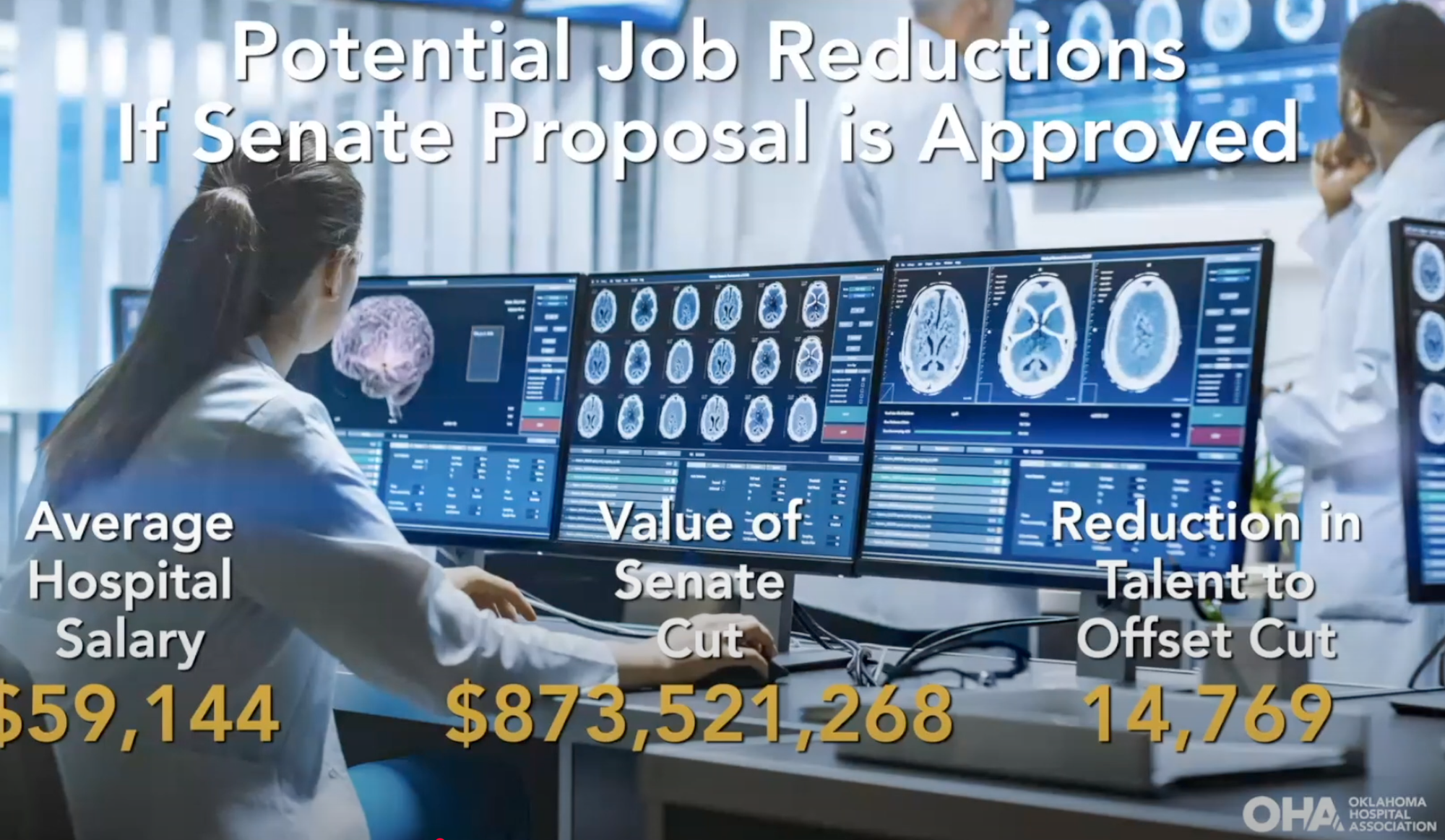
The Oklahoma Hospital Association outlined the potential impacts during a virtual press conference, with leaders from major health systems across the state describing how the cuts could force service eliminations, hospital closures, and workforce reductions exceeding 14,000 full-time positions.
Stillwater Medical Center, which operates hospitals and clinics across 10 communities in north-central Oklahoma, would lose $13 million annually. The health system currently operates with just a 3% operating margin after implementing cost-saving measures following the pandemic.
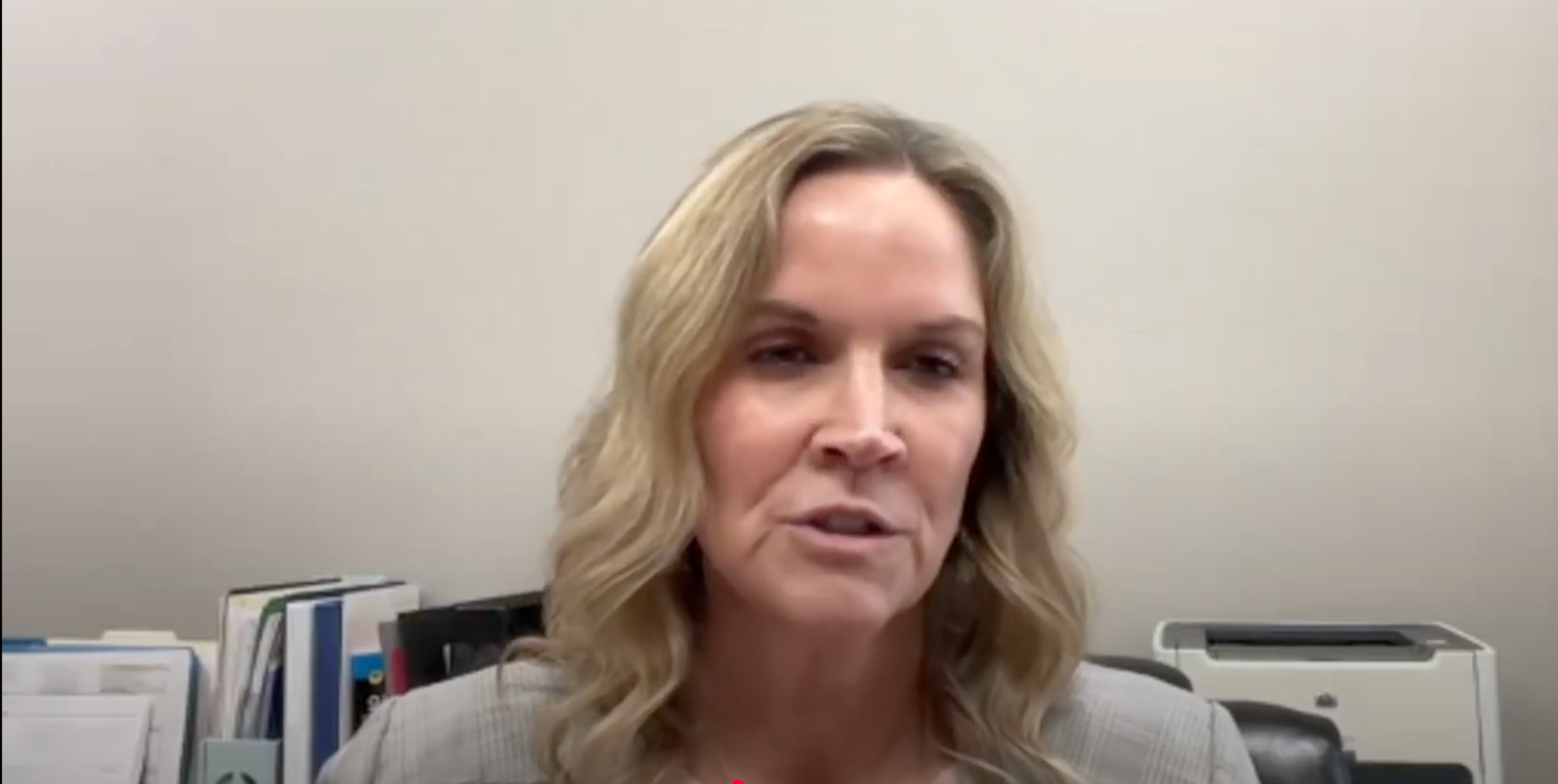
"Prior to the pandemic, we were already feeling huge inflationary pressures," said Denise Webber, president and CEO of Stillwater Medical Center and chair of the Oklahoma Hospital Association. "This would take us to where we would actually lose money."
Webber noted that her organization has worked to preserve rural healthcare by converting struggling hospitals in Perry and Blackwell to rural emergency hospitals, but the proposed cuts would threaten the viability of those facilities.
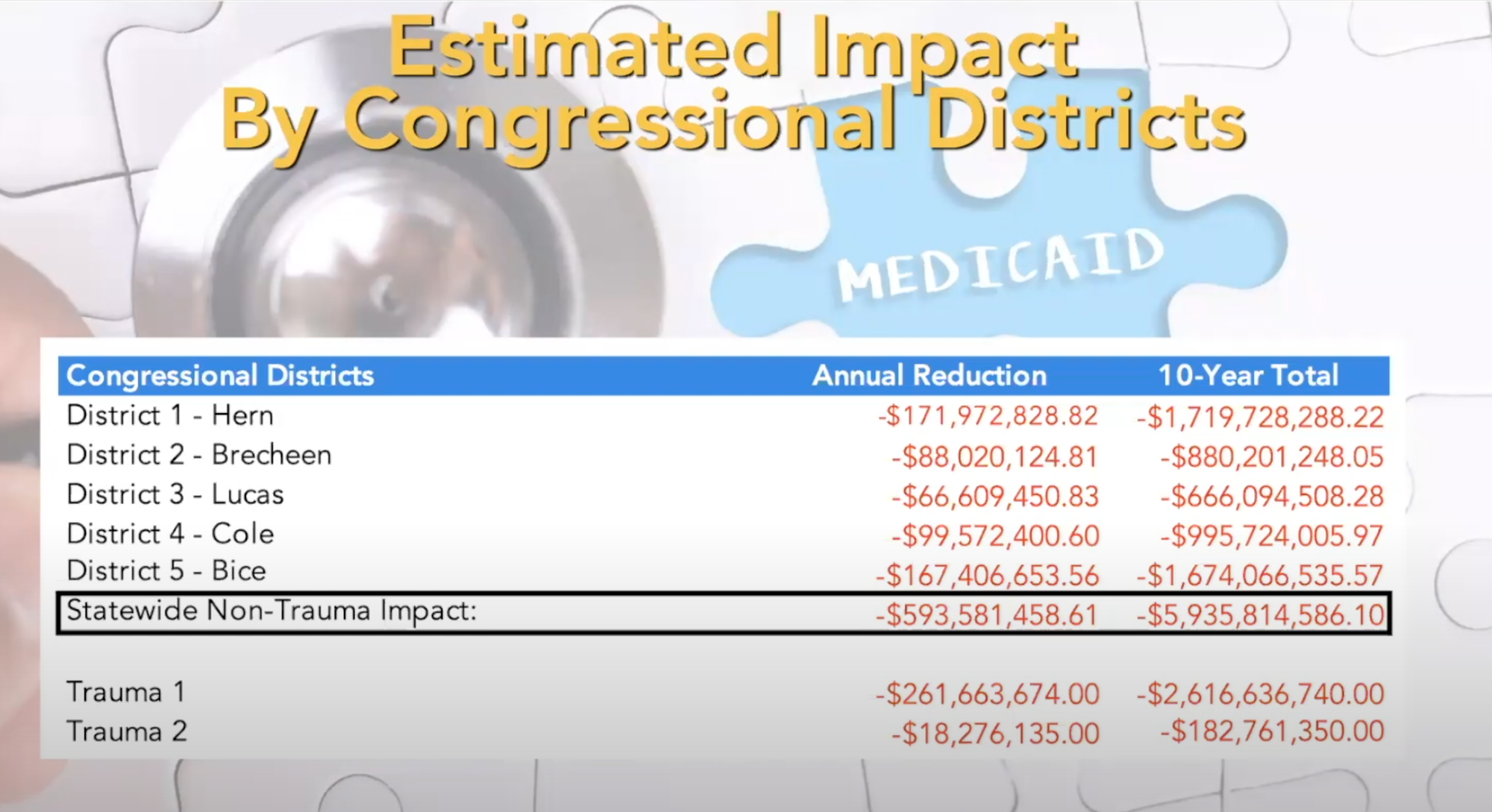
"The total impact of $593 [million] from the PPS hospitals and critical access hospitals. When you add in the impact of Trauma 1, which is OU and Trauma 2, OSU, that's where you come up with the $873 million," said Rich Rasmussen, president of the Oklahoma Hospital Association.
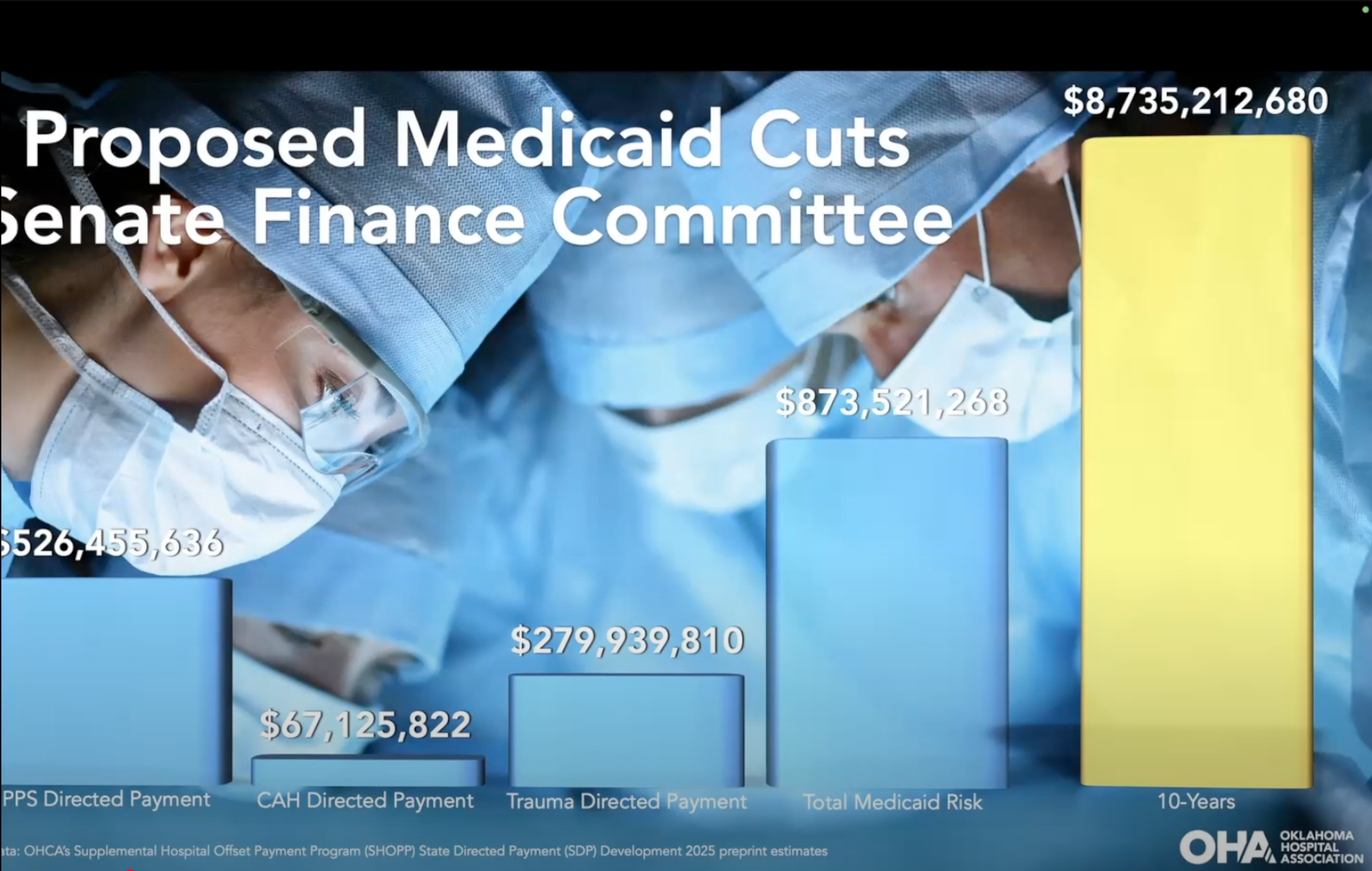
OU Health's University of Oklahoma Medical Center is the state's only Level 1 Trauma Center. – Slides from the Oklahoma Hospital Association's presentation
The proposed cuts target Oklahoma's directed payment program, which currently reimburses hospitals at 90% of average commercial insurance rates for Medicaid patients served through the state's managed care system. The Senate bill would roll back these payments to Medicare rates, creating the $873 million annual shortfall.
Critical access hospitals would face particularly severe impacts, with independent rural facilities potentially seeing their average income reduced by 56%. These hospitals already operate on narrow margins and lose money on Medicare patients, receiving only 99 cents for every dollar of cost to treat Medicare patients.
"The reductions from what we're currently being paid today totals $873 million," Rasmussen said. "If we just did simple napkin math and we said if we had to reduce workforce to equal this Senate cut, it would mean that we would have to reduce our workforce by over 14,000 FTEs."
Childbirth (Obstetrical) services face particular risk, with hospital leaders warning that maternity care could be eliminated in up to 15 northwestern Oklahoma counties. Currently, only 43 of Oklahoma's roughly 165 hospitals deliver babies, with approximately 54% of deliveries in the state covered by Medicaid.
"If Medicaid gets cut this drastically, you're going to see fewer hospitals that deliver babies for all patients," said Bennett Geister, president of Oklahoma City Communities for Mercy and chair-elect of the Oklahoma Hospital Association board. "Over 50% of counties in our state right now are classified as maternity deserts."
Mercy alone would face approximately $100 million in lost funding, potentially affecting over 500 jobs across the state, Geister said.
Sign up for THE STILLWEGIAN
Stillwater Oklahoma's local independent online news. Stay informed with free weekly newsletters.
No spam. Unsubscribe anytime.
Duncan Regional Hospital faces $7 million in cuts, which CEO Jay Johnson said would force the elimination of contract nurses and potentially require caps on patient admissions. The hospital serves as the largest employer in Stevens and Jefferson counties, covering about 50,000 residents in southwestern Oklahoma.
"With these kinds of reductions, there's just no way we could afford that, which would make us have to put an artificial cap on how many patients we could put in our hospital every day," Johnson said
Rural healthcare advocates warn the cuts could force patients to travel significantly farther for care. Trent Bourland, vice president for rural development at SSM Health, said patients may need to travel 40 miles or more for routine care and up to 80 miles for specialty services.
"Rural residents already experience a 20% higher mortality rate compared to our urban populations," Bourland said. "The reductions widen disparities and lead to preventable deaths."
A message from Visit Stillwater
Summer in America's Friendliest College Town calls for live music, kids' camps, livestock shows, art, and so much more. Check out all there is to see and do in The Original Home of Red Dirt Music this month!
The cuts would also eliminate planned expansions in mental health services and other specialty care areas where hospitals were looking to grow using the additional Medicaid funding.
One in four Oklahomans relies on Medicaid for healthcare coverage, with over 60% of Medicaid recipients being women and children. Hospital leaders emphasized that service cuts would affect all patients, not just those covered by Medicaid.
"When you do cut the resources like we're talking about $873 million worth, if a hospital eliminates a service or cuts back on the level of primary care that they can offer because it's just not financially sustainable," Rasmussen said. "They don't eliminate that just for Medicaid patients, that's eliminated for everybody.”
The economic impact extends beyond healthcare, with the 10-year reduction potentially exceeding $25 billion in lost economic activity when accounting for an estimated three to one multiplier effect of healthcare spending in local communities.
Hospital leaders said they have met with Oklahoma's congressional delegation to discuss their concerns but emphasized the need for more time to develop alternatives to the proposed cuts.
"This is happening at such a breakneck speed. There's not ample time to plan and create a strategy that can serve Oklahomans," Webber said. "People who have long relationships with physicians and are receiving care right now may receive something in the mail or a phone call that says you no longer have your doctor, and that is just a travesty."
The cuts would also shift uncompensated care costs to commercial insurance payers, potentially resulting in higher premiums for families across the nation, hospital leaders warned.
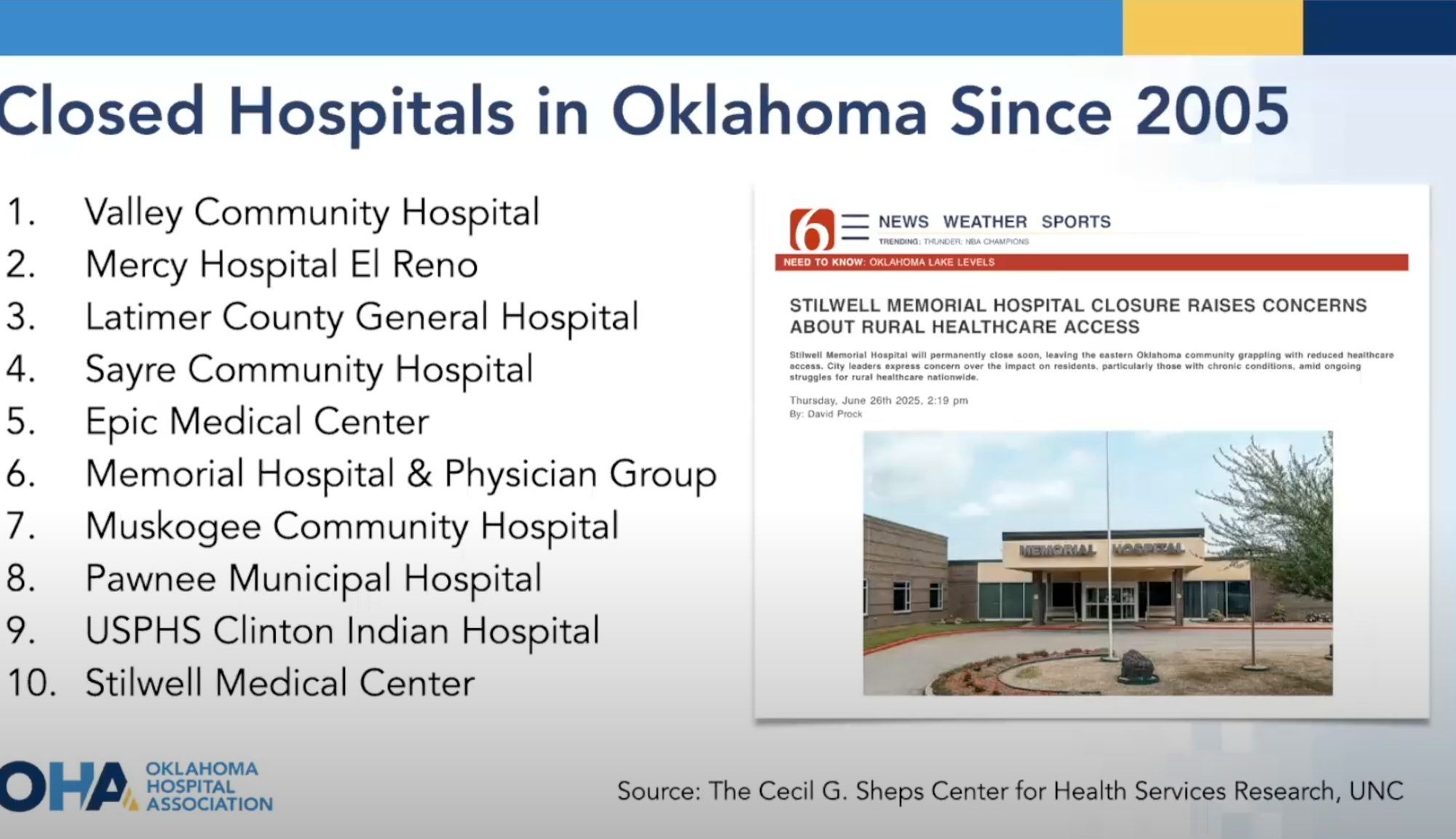
Stilwell Medical Center announced its closure Saturday, becoming the latest addition to a list of more than 20 Oklahoma hospitals that have closed since 2005, highlighting the ongoing challenges facing rural healthcare in the state.
📺 Watch the Oklahoma Hospital Association's presentation